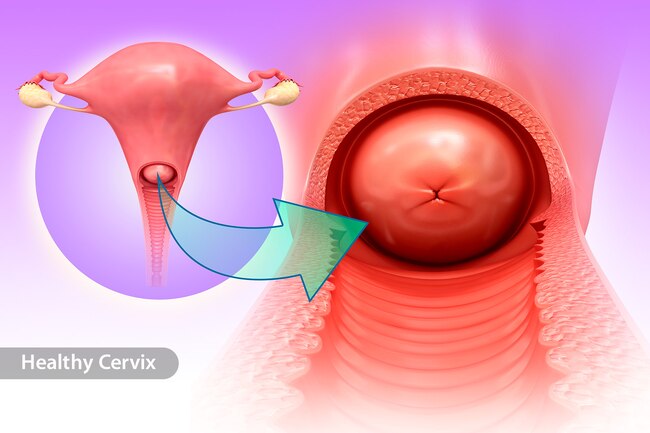
The cervix is part of a woman’s reproductive system. It’s in the pelvis. The cervix is the lower, narrow part of the uterus (womb). Growths on the cervix can be benign or malignant. Benign growths are not cancer. They are not as harmful as malignant growths (cancer).
What is cervical cancer?
Cancer begins in cells, the building blocks that make up tissues. Tissues make up the organs of the body.
Normal cells grow and divide to form new cells as the body needs them. When normal cells grow old or get damaged, they die, and new cells take their place.
Sometimes, this process goes wrong. New cells form when the body does not need them, and old or damaged cells do not die as they should. The build up of extra cells often forms a mass of tissue called a growth or tumor.
Types of cervical cancer
Benign growths (polyps, cysts, or genital warts):
- are rarely a threat to life
- don’t invade the tissues around them
Malignant growths (cervical cancer):
- may sometimes be a threat to life
- can invade nearby tissues and organs
- can spread to other parts of the body
Symptoms of cervical cancer
Studies have found a number of factors that may increase the risk of cervical cancer. For example, infection with HPV (human papillomavirus) is the main cause of cervical cancer. HPV infection and other risk factors may act together to increase the risk even more or can be a cervical cancer sign:
HPV infection: HPV is a group of viruses that can infect the cervix. An HPV infection that doesn’t go away can cause cervical cancer in some women. HPV is the cause of nearly all cervical cancers.
HPV infections are very common. These viruses are passed from person to person through sexual contact. Most adults have been infected with HPV at some time in their lives, but most infections clear up on their own.
Some types of HPV can cause changes to cells in the cervix. If these changes are found early, cervical cancer can be prevented by removing or killing the changed cells before they can become cancer cells. The NCI fact sheet Human Papillomaviruses and Cancer:
- Lack of regular Pap tests: Cervical cancer is more common among women who don’t have regular Pap tests. The Pap test helps doctors find abnormal cells. Removing or killing the abnormal cells usually prevents cervical cancer.
- Smoking: Among women who are infected with HPV, smoking cigarettes slightly increases the risk of cervical cancer.
- Weakened immune system (the body’s natural defense system): Infection with HIV(the virus that causes AIDS) or taking drugs that suppress the immune system increases the risk of cervical cancer.
- Sexual history: Women who have had many sexual partners have a higher risk of developing cervical cancer. Also, a woman who has had sex with a man who has had many sexual partners may be at higher risk of developing cervical cancer. In both cases, the risk of developing cervical cancer is higher because these women have a higher risk of HPV infection.
Stages of cervical cancer
- Stage I: The tumor has invaded the cervix beneath the top layer of cells. Cancer cells are found only in the cervix.
- Stage II: The tumor extends to the upper part of the vagina. It may extend beyond the cervix into nearby tissues toward the pelvic wall (the lining of the part of the body between the hips). The tumor does not invade the lower third of the vagina or the pelvic wall.
- Stage III: The tumor extends to the lower part of the vagina. It may also have invaded the pelvic wall. If the tumor blocks the flow of urine, one or both kidneys may not be working well.
- Stage IV: The tumor invades the bladder or rectum. Or the cancer has spread to other parts of the body.
- Recurrent cancer: The cancer was treated, but has returned after a period of time during which it could not be detected. The cancer may show up again in the cervix or in other parts of the body.
Cervical cancer treatments
- Radical trachelectomy: The surgeon removes the cervix, part of the vagina, and the lymph nodes in the pelvis. This option is for a small number of women with small tumors who want to try to get pregnant later on.
- Total hysterectomy: The surgeon removes the cervix and uterus.
- Radical hysterectomy: The surgeon removes the cervix, some tissue around the cervix, the uterus, and part of the vagina.
- External radiation therapy: A large machine directs radiation at your pelvis or other tissues where the cancer has spread. The treatment usually is given in a hospital or clinic. You may receive external radiation 5 days a week for several weeks. Each treatment takes only a few minutes. Colposcopy is done to illuminate or to magnify the vaginal wall and cervical areas for finding the tumor cells.
- Internal radiation therapy: A thin tube is placed inside the vagina. A radioactive substance is loaded into the tube. You may need to stay in the hospital while the radioactive source is in place (up to 3 days). Or the treatment session may last a few minutes, and you can go home afterward. Once the radioactive substance is removed, no radioactivity is left in your body. Internal radiation may be repeated two or more times over several weeks. Above all HPV cervical cancer vaccine is suggested for children to prevent the HPV viruses and pampolloma viruses. Pap smear is one of the advanced treatment techniques.
Guild lines for prevention
Cervical cancer would also affect girls during teens and these cervical cancer children can consult the doctor if any symptoms are found. Your doctor can describe your treatment choices, the expected results of each, and the possible side effects. You and your doctor can work together to develop a treatment plan that meets your medical and personal needs.
Conclusion
Doctors all over the country are conducting many types of clinical trials (research studies in which people volunteer to take part). They are studying new ways to treat cervical cancer. Hopefully these researches would give a great relief from this deadly disease.